The Heart
Our heart is a two-sided pump. Its function is to guarantee the blood flow between the lungs, where blood is oxygenated, and the body tissues, where oxygen is used as nutriment for the tissues' cells.
HEART CHAMBERS
Our heart is made up of four chambers. The chambers are compartments like small rooms whose function is to store the blood and then push it outside.The two upper chambers, the atria, receive the blood returning into the heart through the veins. The two lower ones, the ventricles, pump the blood to the body through the arteries.
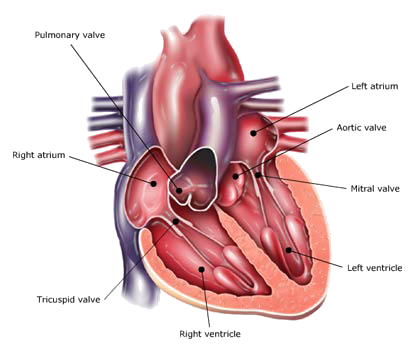
The right atrium receives all the returning blood from the upper and lower parts of the body. It then transfers this blood through the tricuspid valve to the right ventricle, which then pumps it through the pulmonary valve out to the lungs. In the lungs, carbon dioxide is exchanged for oxygen, then the blood returns to the left atrium, which transfers it though the mitral valve into the left ventricle. The left ventricle then pumps the blood through the aortic valve out to the body though the arteries, where the blood supplies tissues with oxygen and removes carbon dioxide. The blood, now depleted of oxygen, is returned to the right atrium by the veins. The left part of the heart needs to exert a stronger force than the right part; therefore the left cardiac walls are thicker and stronger.
HEART VALVES
In our heart we have four heart valves, dividing the four heart chambers. The heart valves are made of two or three leaflets of thin tissue which open and close around 70 times a minute.
The atrioventricular valves separate the upper from the lower chambers; one of these is called the mitral valve, which divides the left atrium and the left ventricle, and the other is the tricuspid valve, found between the right atrium and the right ventricle.
The tricuspid valve is so-called because it has three leaflets, while the mitral valve is called bicuspid, because it has just two leaflets.
The mitral valve has a complex structure. Its cusps are retained by the cordae tendinae, which are linked to the papillary muscles. These structures avoid the prolapse of the valve edge into the atrium.
The outflow valves separate the heart from the two main arteries: the aorta and the pulmonary artery. The aortic valve separates the left ventricle from the aorta, the main artery that carries blood to the body. The pulmonary valve separates the right ventricle from the pulmonary artery. The aortic and the pulmonary valves are said to be semilunar because of their leaflets' shape, which are similar to a half moon. The aortic and pulmonary valves are thin structures, without any muscles; they open and close only thanks to blood pressure gradients.
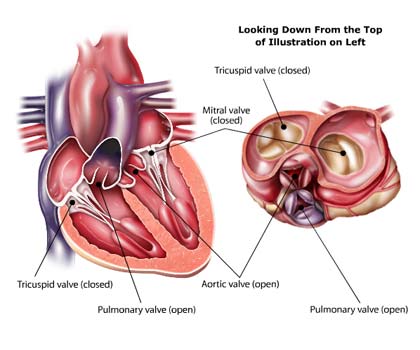
The heart valves close and open in a pulsatile way, filling and emptying the atria and the ventricles. They work as doors, letting in a precise quantity of blood flow in only one direction, and preventing blood backflow. If the blood flows back during the leaflets' closure, the backflow is called regurgitation. If the blood flows back when the leaflets are already closed, this is known as leakage regurgitation. If the heart valve is healthy, there is no regurgitation, neither when the valve is closing, nor when it is closed. Moreover, the valve lets blood flow smoothly, without any turbulence and any blood stasis, which could lead to blood clots.
BLOOD VESSELS
Blood flows in our body through a complex system of tubes. These tubes, called blood vessels, carry blood to and from every part of the body.
Types of blood vessels
Arteries
Blood vessels which carry oxygenated blood from the heart to the various part of the body.
Capillaries
Capillaries connect arteries to veins. Capillaries are the smallest of a body's blood vessels and are important for the interchange of oxygen, carbon dioxide, and other substances between blood and tissue cells.
Veins
Blood vessels which carry low oxygenated blood from the various part of the body to the heart.
Coronary Artery Disease
Coronary artery disease (CAD), also referred to as coronary heart disease, is a chronic disease caused by narrowed coronary arteries that limit the blood and oxygen flows to the heart. Coronary artery disease is the most common type of heart disease and it is one of the leading causes of death in both men and women in United States and Europe.
Coronary arteries constantly supply your heart with blood, oxygen and nutrients. When the arteries become narrowed or clogged and can’t supply enough blood to your heart, the result is coronary artery disease. Blood clot formation causes the coronary arteries to narrow, reducing blood flow. When one of the coronary arteries becomes severely or totally blocked, usually by a blood clot, the result can be a heart attack, also known as myocardial infarction. The part of the heart muscle that is not receiving the oxygen-rich blood that it needs, it will begin to die and some of the heart muscle may become permanently damaged.
Causes of Coronary Artery Disease
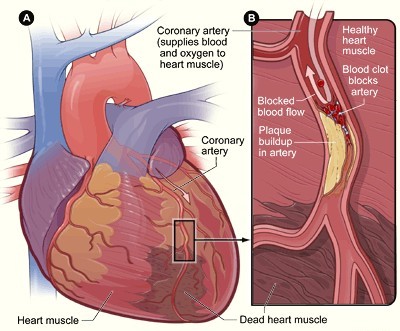
Coronary artery disease is caused by the narrowing or blockage of the coronary arteries caused by atherosclerosis, a condition known also as "hardening of the arteries." Atherosclerosis is a chronic inflammatory response in the walls of arteries. It is the build up of cholesterol and fatty deposits, called plaques, on the inner wall of the arteries.
Atherosclerosis is gradual, often taking decades before the affected person is in danger of cardiovascular problems. As a plaque builds up, blood vessels gradually harden and narrow, and this can affect the flow of blood through the artery. Without adequate blood, the heart becomes starved of oxygen and the vital nutrients it needs to work properly. Ultimately, if one or more arteries become completely blocked, heart tissue will die, resulting in heart attack.
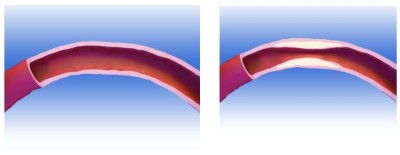
Healthy coronary arteries are shaped like hollow tubes with smooth and elastic walls. Unhealthy or diseased arteries are stiff or hardened and present obstructions (plaques) that can interfere with normal blood flow.
The abnormal narrowing or obstruction in a blood vessel is called stenosis. The narrowing of the artery, because of the presence of plaques, restricts blood flow. Over time the plaque may calcify, reducing artery’s ability to expand and contract and narrows the artery, reducing the amount of blood that can flow through it. As a consequence, tissues supplied by the affected artery don’t receive enough blood and heart does not receive enough oxygen to work properly.
If one of these plaque deposit ruptures a blood clot can rapidly form and completely block the vessel. If the vessel is a coronary artery, it can lead to a heart attack.
Coronary Artery Disease Risk Factors
Although the exact cause of hardening of the arteries in not known, atherosclerosis is usually caused by high cholesterol. High blood pressure, diabetes and smoking can also contribute to coronary artery disease. Physical inactivity and obesity are other factors that can lead to coronary artery disease.
Coronary Artery Disease Symptoms
Patients suffering from coronary artery disease can experience regular episodes where the heart is not receiving enough oxygen-rich flow (Cardiac ischemia). Symptoms of coronary artery disease can range from mild to severe. The most common symptom of coronary artery disease is angina pectoris, also referred to as chest pain. Other symptoms include sense of heaviness, fatigue, shortness of breath, unexplained sweating, uneven or rapid heartbeats, weakness, dizziness, or loss of consciousness. If the patient feels no symptoms, this is called silent ischemia.
Unfortunately, some people have coronary artery disease or even heart attacks without ever experiencing any of these symptoms. This can be especially true for people with diabetes.
Signs and symptoms of heart attack
Heart attack
It is a medical condition that occurs when blood flow to a section of heart muscle becomes blocked, most commonly due to rupture of a vulnerable plaque. Heart attack is also known as myocardial infarction (AMI or MI), because part of the heart muscle (myocardium) may literally die (infarct). If the flow of blood isn’t restored quickly, the section of heart muscle becomes damaged from lack of oxygen and begins to die.
Signs and symptoms of heart attack
Chest pain is the most common symptom of acute myocardial infarction and is often described as a sensation of tightness, pressure, or squeezing. It can be mild or severe. Other common symptoms of heart attack include upper body discomfort, shortness of breath, nausea vomiting or dizziness. The symptoms of angina can be similar to the symptoms of a heart attack. Angina usually lasts for only a few minutes and goes away with rest. Angina that doesn’t go away or changes from its usual pattern (occurs more frequently or occurs at rest) can be a sign of the beginning of a heart attack.
Treatment of Heart Attack
Early treatment can prevent or limit damage to the heart muscle. Once the diagnosis of heart attack is confirmed or strongly suspected, treatments to try to restore blood flow to the heart are started as soon as possible. Treatments include medications and medical procedures.
Diagnosis of coronary artery disease
The diagnosis of coronary artery disease is based on patient’s symptoms, personal, family and medical history. The General Practitioner will listen to the description of your symptoms and will carry out a physical examination. If your General Practitioner thinks something should be investigated in greater depth, he may refer you to a cardiologist in order to conduct more specific tests, such as:- Blood tests. Blood tests can detect the amount of some markers in the bloodstream, which are released during a heart attack. Higher than normal levels of these proteins in the bloodstream is evidence of a heart attack. Commonly used blood tests include troponin tests, CK or CK-MB tests, and serum myoglobin tests.
- An echocardiogram. This test uses sound waves to produce images of the inside of patient’s heart
- Chest x-ray
- An electrocardiogram (ECG). This test detects and records the electrical activity of the heart. The highly sensitive electrocardiograph machine detects heart’s irregularities, disease and damage by measuring the heart’s rhythm and electrical impulses.
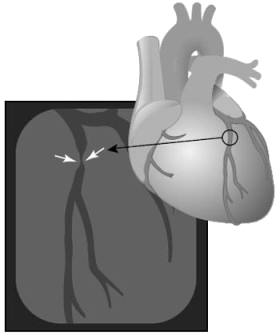
- Coronary angiography. Coronary angiography is a procedure using x-rays to examine the heart and blood vessels and is part of a procedure called cardiac catheterization. Cardiac catheterization is an invasive procedure imaging that allows the evaluation of the heart functioning. A long, narrow tube called catheter is inserted trough a plastic introducer sheath. Then the catheter is guided through the blood vessels and advanced up to the coronary arteries with the aid of an x-ray machine. A contrast dye that can be detected on x-ray is injected into the blood stream trough the tip of the catheter. The x-ray machine then takes a series of images (angiograms), producing a detailed look of the inside of the heart. If the angiograms show the presence of a stenosis, which cannot be treated with oral medications, then another procedure, called angioplasty, may be used to restore the blood flow trough the artery.
Treatments of coronary artery disease
There are three ways to treat atherosclerotic disease: medications, minimally invasive interventional procedures such as percutaneous transluminal coronary angioplasty (PTCA), stent implantation, and surgery.
Medical therapy
Most patients with heart disease receive medication to help prevent a heart attack. A number of different kinds of medicines may be used to treat heart attack.
-
Thrombolytic medicines are used to dissolve blood clots that are blocking the coronary arteries.
-
Beta Blockers decrease the workload on the heart. Beta blockers also are used to relieve chest pain or discomfort and to help prevent additional heart attacks. Beta blockers also are used to correct arrhythmias (irregular heartbeats).
-
Angiotensin-Converting Enzyme (ACE) Inhibitors lower blood pressure and reduce the strain on the heart. They also help slow down further weakening of the heart muscle. Anticoagulants thin the blood and prevent clots from forming in your arteries.
-
Antiplatelets (such as aspirin and clopidogrel) stop platelets (a type of blood cell) from clumping together and forming unwanted clots.
While medications do not eliminate the narrowing of arteries, they can help improve the efficiency of the heart and reduce symptoms such as chest pain (angina).
PTCA (Percutaneous Transluminal Coronary Angioplasty)
Coronary angioplasty (also called percutaneous coronary intervention PCI) is a medical procedure used to restore blood flow through coronary arteries that are narrowed or blocked by a blood clot.
Stents have been used to treat coronary artery disease (CAD) for over two decades. Nowadays, it's common to insert a stent to keep a coronary artery open and maintain blood flow after an angioplasty. Each year, more than 2 million people receive a stent.
Stenting is a minimally invasive procedure where a stent and balloon are used together to push back plaque deposits inside a coronary artery to treat heart disease.
A coronary stent is a small, expandable mesh tube made of medical-grade stainless steel or cobalt alloy. These stents help reduce the chance of the artery becoming blocked or narrowed again after an angioplasty. Once implanted, the stent stays in the artery permanently.
The Stent Procedure:
During an angioplasty, the stent is placed on a small balloon that is inflated inside the coronary artery to push back plaque and restore blood flow. Once the plaque is compressed against the artery wall, the stent expands and acts as a scaffold to keep the artery open. The balloon is then deflated and removed, leaving the stent in place. Sometimes, more than one stent may be needed depending on the blockage length.
Stents are beneficial because they provide permanent support to the artery, helping to prevent it from narrowing again, although this can still happen.
Drug-Eluting Stents:
Some newer stents have a medicated coating to help prevent the artery from narrowing again. Both bare metal and drug-eluting stents can effectively reopen coronary arteries. However, drug-eluting stents (DES) are often more effective at keeping the artery open over time.
While stents are generally safe and effective, there is a rare risk of stent thrombosis, where a blood clot forms at the stent site. This can block blood flow and potentially cause a heart attack or death. Stent thrombosis can occur with both bare-metal and drug-eluting stents. Researchers are studying whether certain drug-eluting stents have a higher risk of this complication.
The most important thing you can do is follow your cardiologist's advice on taking anticlotting medication, known as dual antiplatelet therapy (aspirin with clopidogrel or ticlopidine). It's crucial not to stop this medication without your cardiologist's approval.
CABG
Coronary artery bypass grafting is a surgery in which arteries or veins are taken from other areas the body and sewn in place to bypass blocked coronary arteries providing a new route for blood flow to the heart muscle.
GLOSSARY
Angina pectoris
Commonly known as angina, is chest pain due to ischemia (a lack of blood and hence oxygen supply) of the heart muscle, generally due to obstruction or spasm of the coronary arteries.
Angiography
Procedure in which radiopaque dye is injected into the circulatory system in order to visualize the coronary arteries.
Angioplasty
Is the mechanical widening of a narrowed or totally obstructed blood vessel.